Acute Vestibular Syndrome: Important Role of HINTS-Plus Exam
Acute Vestibular Syndrome (AVS) is characterized by sudden onset of dizziness or vertigo, often accompanied by nausea, vomiting, and gait instability. Given the overlap in symptoms between benign and life-threatening causes, accurate diagnosis is critical. The evolution of bedside tests like HINTS (Head-Impulse, Nystagmus, and Test of Skew) and HINTS Plus (add finger rub test) offers clinicians a valuable toolkit to distinguish central causes of vertigo, such as stroke, from peripheral vestibular dysfunction. Recent research has delved into the effectiveness of these tests, highlighting their potential in improving patient outcomes.
The Evolution of HINTS Plus
Initially developed as HINTS, this series of three simple bedside tests—Head Impulse Test (HIT), Nystagmus, and Test of Skew—has proven effective in differentiating central from peripheral vestibular causes in AVS, which is 96% specific and 100% Sensitive in identifying a central cause of AVS. However, the addition of a fourth test, focusing on audiological signs, resulted in the development of HINTS Plus. This advancement has been pivotal in detecting accompanying hearing loss, which is often linked to stroke.
In their 2023 review, Carmona et al. highlighted that while HINTS remains a robust diagnostic tool, HINTS Plus adds another layer of accuracy. Stroke-related AVS can be difficult to catch, especially in smaller or more subtle cases. By adding a bedside hearing test (typically finger rub or tuning fork tests), clinicians can screen for hearing loss, which may indicate central causes, such as posterior circulation strokes.
A Critical Analysis of HINTS Plus
A comprehensive review by Orinx et al. (2022) explored the movement from HINTS to HINTS Plus, emphasizing its practicality in clinical settings. They argue that HINTS Plus provides a superior framework for distinguishing between benign peripheral vestibular disorders (such as vestibular neuritis) and more serious central pathologies. The hearing loss component was particularly beneficial in challenging cases, offering a more nuanced approach to identifying stroke.
Their findings suggest that HINTS Plus significantly reduces the risk of misdiagnosis, especially in patients presenting with subtle symptoms. They found that the test's sensitivity and specificity for detecting central causes of AVS increased with the addition of the auditory assessment, making it a gold-standard tool in emergency medicine for clinicians managing dizzy patients.
Positive Criteria (Suggesting Central Cause, e.g., Stroke) – Positive criteria are met if at least ONE of the four tests is positive.
Head-Impulse Test (HIT)
Normal: The patient’s eyes stay fixed on the target despite a rapid head movement (i.e., no corrective saccade). This suggests a central lesion.
A normal head-impulse test is suspicious for stroke.
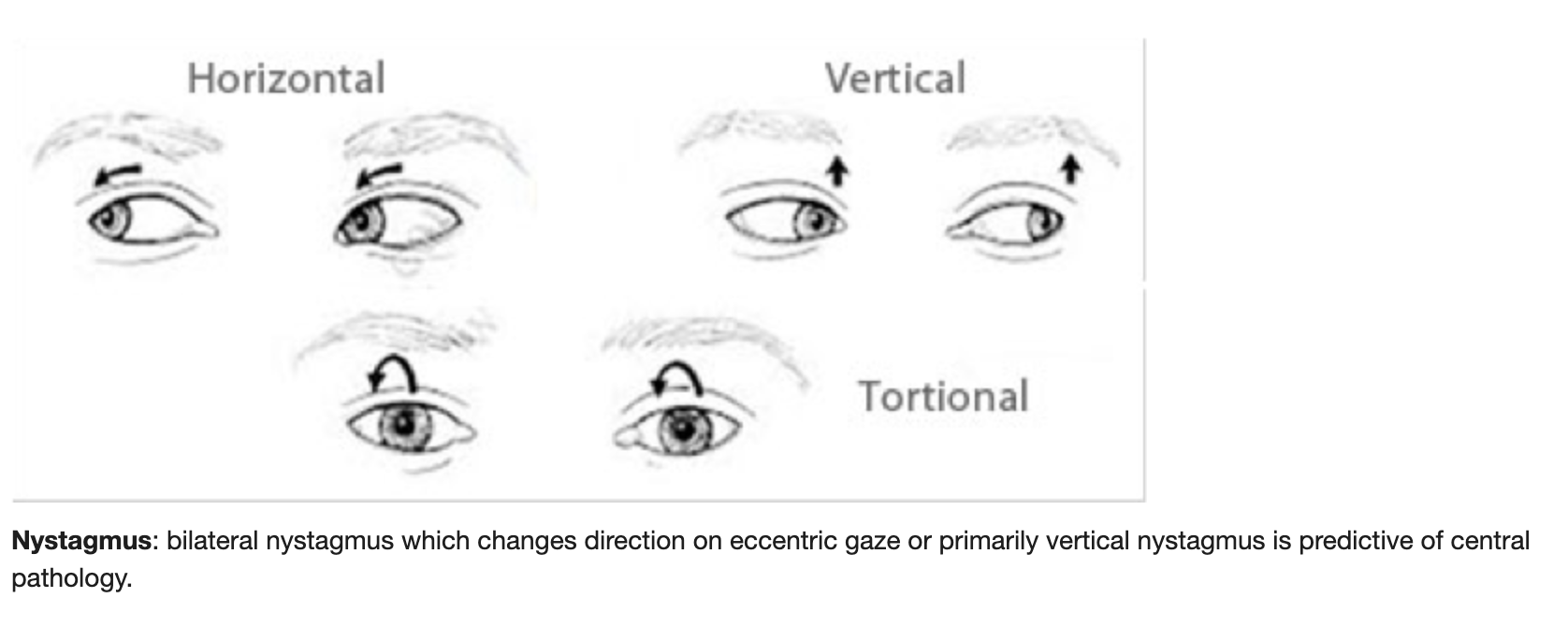
2. Nystagmus
Direction-changing nystagmus: When the fast phase of nystagmus changes direction depending on the gaze direction (e.g., left-beating nystagmus when looking left, right-beating when looking right).
This pattern is suggestive of a central cause, such as stroke.
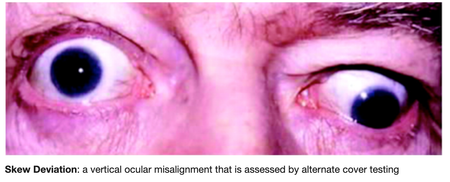
3. Test of Skew (Vertical Skew Deviation)
Positive: Cover one eye and when uncovered, the covered eye jumps vertically to realign with the other eye. This indicates a vertical misalignment, suggesting a brainstem or cerebellar lesion.
4. Hearing Test (Plus Component)
Hearing loss: If the patient presents with new, unexplained hearing loss (usually tested with finger rub or tuning fork test), this can suggest a central cause, particularly if the hearing loss is unilateral and accompanies vertigo or dizziness.
Negative Criteria (Suggesting Peripheral Cause, e.g., Vestibular Neuritis) – Must meet all criteria in order to be negative.
Head-Impulse Test (HIT)
Abnormal: A corrective saccade (a quick eye movement) occurs when the head is turned rapidly toward the side of the lesion (the patient’s eyes lose focus on the target and then "jump" back to it). This finding is consistent with peripheral vestibular dysfunction, such as vestibular neuritis.
Nystagmus
Unidirectional nystagmus: The fast phase of nystagmus beats in the same direction regardless of the gaze direction (e.g., always left-beating). This finding typically indicates a peripheral vestibular cause.
Test of Skew (Vertical Skew Deviation)
Negative: No vertical correction is needed when alternating the covering of each eye. The absence of skew deviation points toward a peripheral cause of the dizziness.
Hearing Test (Plus Component)
No hearing loss: The absence of new hearing loss suggests a peripheral cause, such as vestibular neuritis, where hearing is typically unaffected.
Conclusion: The Critical Role of HINTS Plus
The diagnostic challenge of acute vestibular syndrome (AVS) in both primary care and emergency settings underscores the value of the HINTS Plus exam. By significantly improving diagnostic precision, especially for stroke-related dizziness, this tool has the potential to save lives and enhance patient outcomes. Adding an auditory assessment component extends the test’s utility in identifying central causes of vertigo, offering a simple yet effective method for detecting potentially life-threatening conditions like stroke.
As future advancements bring new diagnostic markers and technologies, HINTS Plus remains an essential part of the clinician's repertoire for evaluating AVS. Mastery of this test equips healthcare providers with the evidence-based tools needed for rapid and accurate decision-making, ensuring better care in high-stakes environments.
Positive HINTS Plus findings (e.g., normal head-impulse, direction-changing nystagmus, skew vertical deviation, and hearing loss) suggest a central cause, like stroke.
Negative HINTS Plus findings (e.g., abnormal head-impulse, unidirectional nystagmus, no skew, no hearing loss) point to a peripheral cause, such as vestibular neuritis.
These distinctions enable clinicians to quickly identify the source of acute dizziness and vertigo, ensuring prompt and effective treatment, particularly in emergency settings.
References: